Hysterectomy continues to be one of the most common surgical procedures among women in the United States, with over 600,000 operations performed each year.
Estrogen drop accelerates bone breakdown and slows bone formation, making postmenopausal women especially vulnerable to osteoporosis.
As of 2021, approximately 14.6% of women aged 18 and older had undergone a hysterectomy. The prevalence rises significantly with age, exceeding 40% among women aged 75 and older. While the procedure can offer essential relief from various gynecological conditions, understanding its long-term impact — particularly on bone health — is crucial.


When the ovaries are removed during a hysterectomy (a procedure known as oophorectomy), estrogen levels plummet, triggering early menopause. Even if the ovaries are left intact, changes in blood supply can still impair hormone production, subtly affecting bone strength over time. It is essential for women considering or recovering from a hysterectomy to be informed about these risks and to adopt strategies that promote strong, healthy bones.
Why Osteoporosis Occurs
Osteoporosis occurs more frequently in women due to biological and hormonal factors that influence bone density throughout life. Women naturally have smaller, thinner bones and lower peak bone mass compared to men, which means they start with less bone “in reserve” as they age. Estrogen, a hormone that plays a key role in maintaining bone strength, declines sharply during menopause. This hormonal drop accelerates bone breakdown and slows bone formation, making postmenopausal women especially vulnerable to osteoporosis. Additionally, women who experience early menopause or undergo oophorectomy face an even greater risk due to the sudden loss of estrogen.
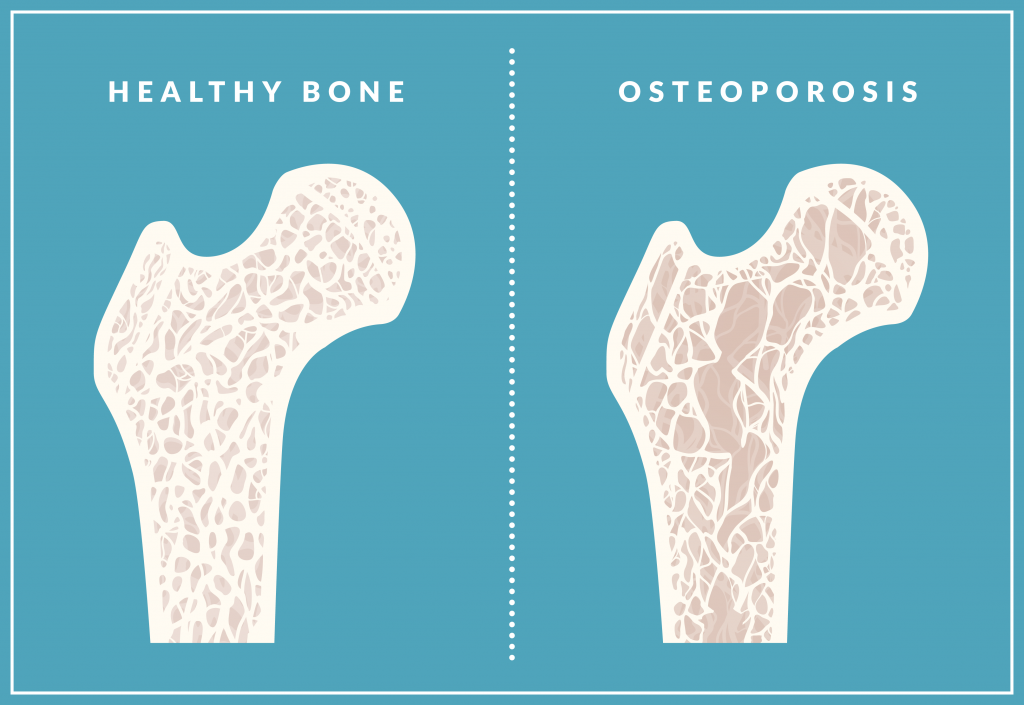
Other contributing factors include lifestyle, genetics, and certain medical conditions. Women with a family history of osteoporosis, low calcium intake, or sedentary habits are more likely to develop the disease. Conditions such as thyroid disorders, eating disorders, and autoimmune diseases can also interfere with bone metabolism. Long-term use of medications like corticosteroids or certain cancer treatments may further weaken bones.
How to Strengthen Bone Health
After a hysterectomy — especially if it involved the removal of the ovaries — prioritizing bone health becomes essential. Here are several effective strategies for strengthening bones and maintaining skeletal health post-surgery:
- Weight-bearing exercises – Activities like walking, dancing, stair climbing, and resistance training help stimulate bone growth and improve balance, reducing fracture risk.
- Calcium and vitamin D – Aim for at least 1,200 mg of calcium daily and ensure adequate vitamin D through sunlight, diet, or supplements to support calcium absorption.
- Healthy diet – Focus on leafy greens, dairy, legumes, and fortified foods. Avoid excessive caffeine and alcohol, which can weaken bones.


- Hormone replacement therapy (HRT) – In some cases, doctors may recommend HRT to help maintain estrogen levels and slow bone loss.
- Lifestyle choices – Quit smoking, limit alcohol, and maintain a healthy weight to support overall bone health.
- Bone density screening – Regular scans can detect early signs of osteoporosis and guide treatment decisions.
Conclusion
A hysterectomy can be life-changing for women suffering from chronic gynecological issues such as uterine fibroids, endometriosis, abnormal bleeding, or uterine prolapse. The procedure often results in significant relief, allowing women to regain control over their health and well-being. In cases involving cancer or increased risk of cancer, hysterectomy may be both preventive and lifesaving. Many women experience improved emotional and physical health following surgery.


While the benefits of hysterectomy can be substantial, it’s important to acknowledge and prepare for its long-term impacts on bone health. By incorporating regular exercise, a calcium-rich diet, vitamin D, and healthy lifestyle habits, women can build and maintain stronger bones. These proactive measures foster resilience, promote independence, and support quality of life well into the future.
