Imagine being in a busy city, with sounds all around.
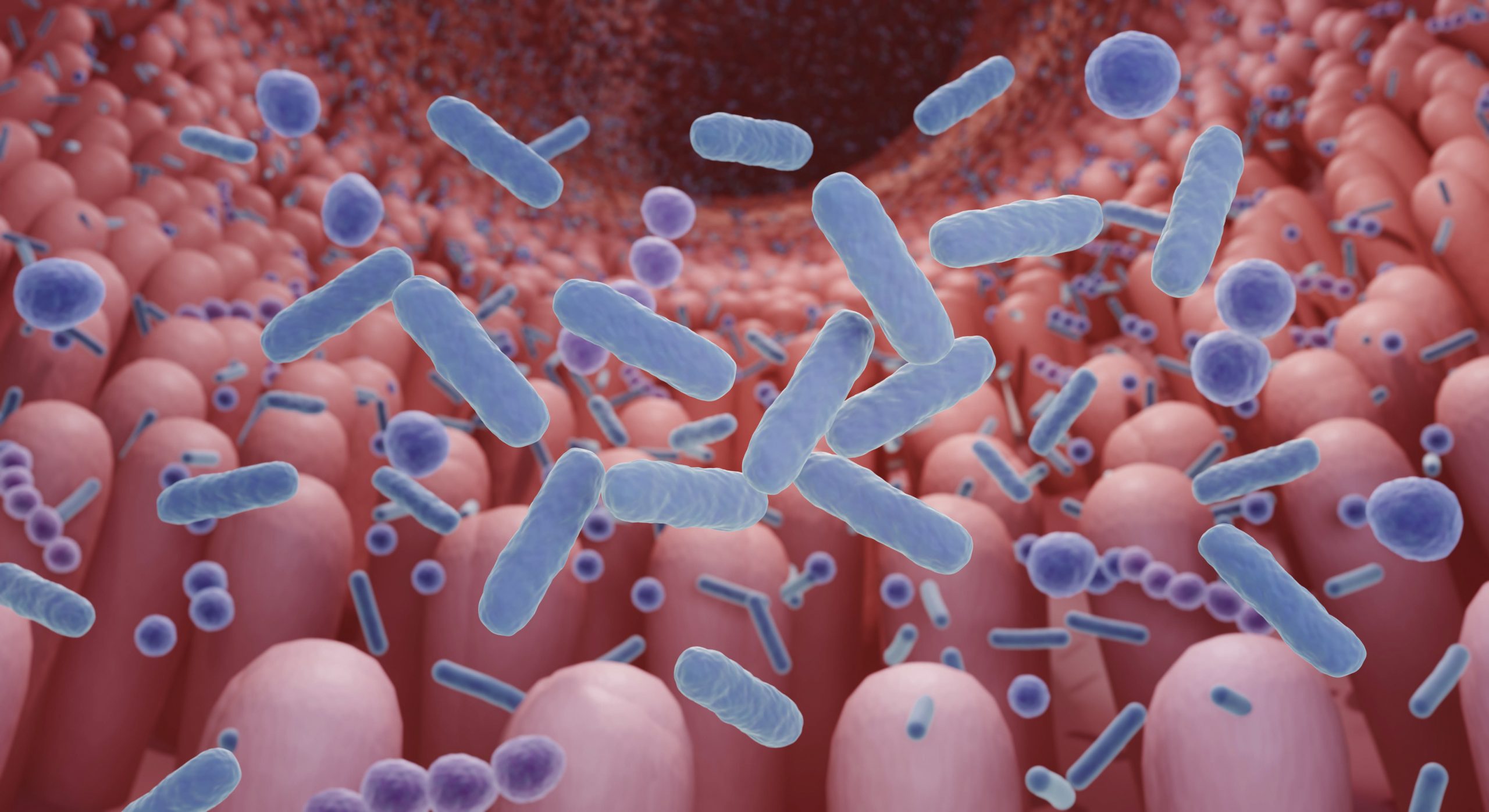
But for some, there’s another layer to this world — a place where voices are heard and things appear that aren’t really there. This is life for those with schizophrenia, a complex and often misunderstood mental health condition.
What is Schizophrenia?
Schizophrenia is not a split personality, as some might believe, but rather a chronic brain disorder that affects how a person thinks, feels, and behaves. It often manifests in hallucinations, delusions, and disorganized thinking. Imagine your mind as a puzzle — schizophrenia jumbles the pieces, making it challenging to make sense of the world. Schizophrenia affects approximately 24 million people or 1 in 300 people (0.32%) worldwide. Onset is most often during late adolescence and the twenties, and tends to happen earlier among men than among women.
Warning Signs
Recognizing the warning signs of schizophrenia can be crucial for early intervention and support. Keep an eye out for:
- Hallucinations: Hearing voices or seeing things that aren’t there.
- Delusions: Firmly held beliefs that are not based in reality, such as paranoia or grandiosity.
- Disorganized Thinking: Difficulty organizing thoughts or connecting ideas in a logical way.
- Social Withdrawal: Pulling away from friends, family, and social activities.
- Unusual Behavior: Acting in ways that are erratic, bizarre, or unpredictable.
How to Get Help
If you or someone you know is experiencing symptoms of schizophrenia, it’s essential to reach out for support. Often, these services are covered by insurance. Here’s what you can do:
- Talk to a Healthcare Professional: Start by discussing your concerns with a doctor or mental health professional. They can provide an evaluation and recommend appropriate treatment options.
- Explore Therapy: Therapy, such as cognitive-behavioral therapy (CBT), can help manage symptoms and improve coping skills.
- Medication Management: Antipsychotic medications are often prescribed to help alleviate symptoms of schizophrenia. It’s essential to work closely with a healthcare provider to find the right medication and dosage.
- Build a Support Network: Surround yourself with understanding friends, family, or support groups who can offer encouragement and empathy on your journey.
Schizophrenia may cast shadows over one’s reality, but with understanding, recognition, and support, there is light to be found. Remember, you are not alone — reach out, seek help, and embark on a path towards brighter days ahead.
2 out of 3 people suffering from psychosis never receive the proper healthcare they need to treat their illness, including those with schizophrenia.