Every revolution in medicine begins with a discovery that seems small at first.
For GLP-1, that discovery was a hormone quietly produced in the gut, released after meals to help the body manage energy. Today, GLP-1s are no longer obscure — they’re reshaping how we think about diabetes, weight, heart health, and more.
GLP-1, short for glucagon-like peptide-1, is a natural hormone that plays a critical role in digestion and metabolism. When food enters the stomach, GLP-1 is released, sending signals to the pancreas, liver, and brain. It tells the pancreas to release insulin only when blood sugar is high, suppresses glucagon so the liver doesn’t flood the bloodstream with sugar, and slows digestion so you feel fuller longer. Pharmaceutical science has harnessed this natural process, creating GLP-1 medications that mimic and extend the hormone’s effects.
What Are the Benefits?

The impact of GLP-1s is wide-ranging. They improve blood sugar control, making them a cornerstone therapy for type 2 diabetes. They reduce appetite by slowing stomach emptying, which often leads to meaningful weight loss. They also influence the brain’s appetite centers, dialing down cravings and helping people feel satisfied with less food.
But the benefits don’t stop there. GLP-1s have been shown to lower the risk of cardiovascular events like heart attacks and strokes, improve cholesterol and triglyceride levels, and even show promise in protecting kidney health. Over time, consistent use can reduce complications tied to chronic disease, offering not just short-term relief but long-term outcomes. Recent studies have shown promising results for treatment for chronic pain, inflammation, and addiction recovery due to how GLP-1s affect brain signals.
How Do GLP-1s Work?
Think of GLP-1s as conductors of a metabolic orchestra. They cue the pancreas to release insulin only when it’s needed, preventing dangerous spikes or drops in blood sugar. They quiet the liver’s tendency to overproduce sugar, keeping levels steady. They slow the digestive process, stretching out satiety and reducing overeating. And they act directly on the brain, influencing appetite regulation in ways that make healthy choices easier to sustain.

How Do You Use GLP-1s?

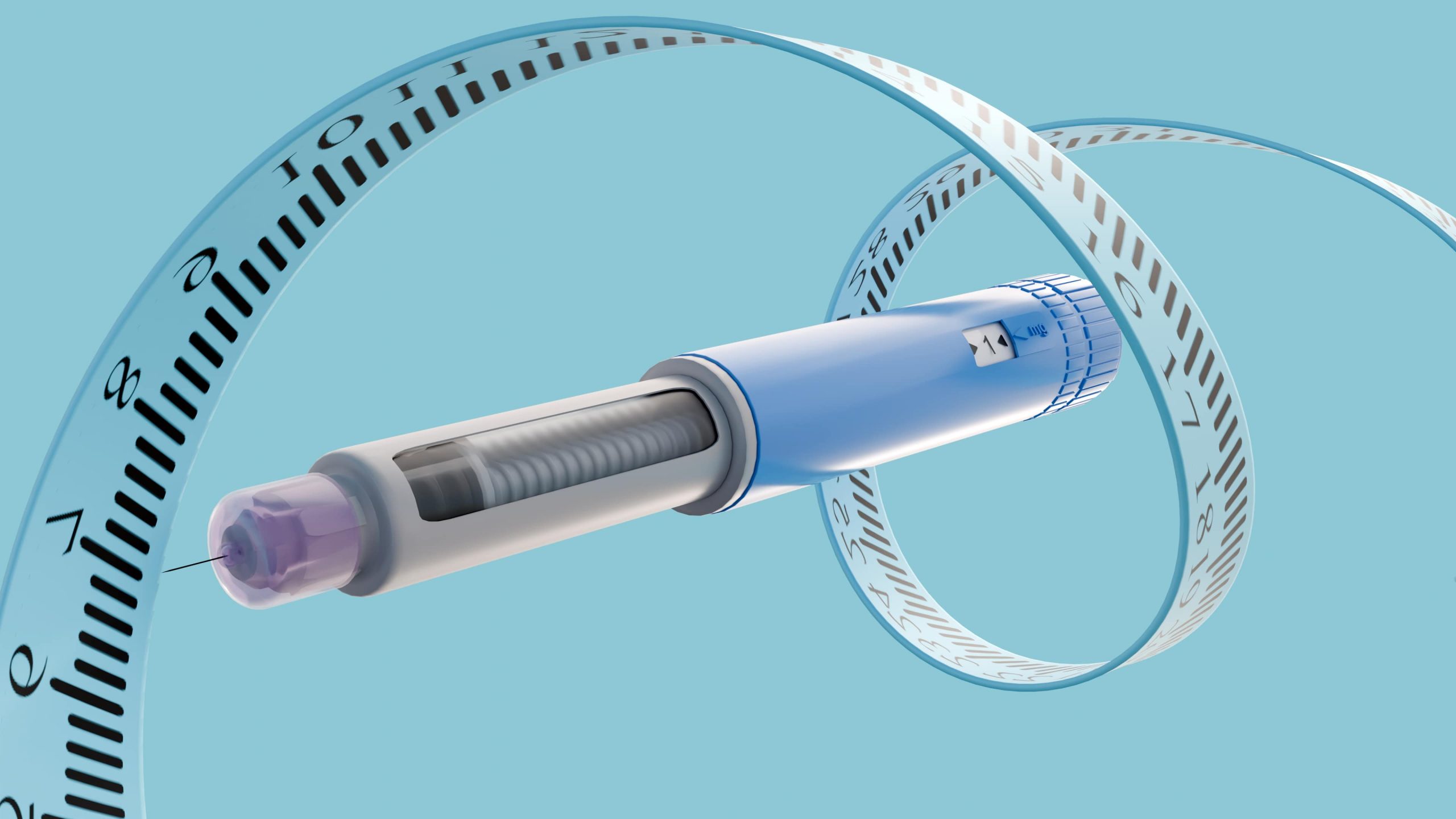
GLP-1 medications come in both injections and pills, depending on the formulation. Some are taken daily, while others are designed for weekly use, offering flexibility for different lifestyles. They’re most effective under medical supervision, since dosing and monitoring are essential. Pairing GLP-1s with healthy eating with plenty of protein and fiber and regular exercise with a focus on strength training amplifies their benefits, turning them into powerful allies in a holistic health plan.
Like any therapy, they come with considerations. Side effects such as nausea or gastrointestinal discomfort are common early on but often fade with time. Other common side effects include headaches, muscle loss, and hair loss. They aren’t suitable for everyone — those with certain medical histories, like pancreatitis, may need alternatives.
And consistency matters; the benefits build gradually over weeks and months, not overnight.
GLP-1s are not magic bullets, but they are remarkable tools. They work best as part of a broader approach to health, complementing lifestyle changes and other therapies. What makes them so exciting is their ability to harness the body’s own biology — transforming a natural hormone into a modern medical breakthrough.
The story of GLP-1s is one of science uncovering the hidden power of the body’s signals. From a quiet hormone in the gut to a global movement in medicine, GLP-1s prove that sometimes the smallest discoveries can spark the biggest revolutions. They offer balance, health, and hope — not as miracles, but as evidence that biology itself can be our greatest ally.