We have so many options for medical care these days that it is important to understand the types of care, when it’s appropriate for each type, the impacts on the time it may take to get care, and how much that care may cost.
Nurse Lines – This is a great resource if you need a quick answer to a health issue that doesn’t require immediate medical treatment. They are typically free as a part of your medical insurance and available 24/7. Nurse Lines can answer questions about your symptoms, self-care/home treatments, medications and side effect, and can help you decide when to seek care.
Telemedicine – This resource can be used when you need care for minor illnesses and aliments but would prefer not to or cannot leave home since they are offered by phone or online if you have access to a webcam. Some telemedicine visits can even be scheduled outside of normal doctor’s hours. There are usually copays or flat fees for these types of visits, but they often give you immediate access to care and in some cases in some states can provide prescriptions. Best used for cold & flu symptoms, bronchitis, urinary tract infections, and sinus infections.
Primary Care Center – Use this resource for routine care or treatment of current health issues. Your primary care doctor knows you and your health history and can provide help with most of your care and prescription needs. Appointments usually are required and can come with wait time once in the office. Copays and/or coinsurance typically applies. Use your primary care center for routine checkups, immunizations, preventive services, and managing your general health.
Urgent Care Center – This resource is used when you need care quickly but is not a true emergency. They offer treatment for non-life-threatening injuries and illnesses like strains, sprains, minor broken bones, and minor infections or burns. These visits are subject to copay and/or coinsurance and can be more costly that a primary care center visit. Walk-ins are welcome but may have long wait times.
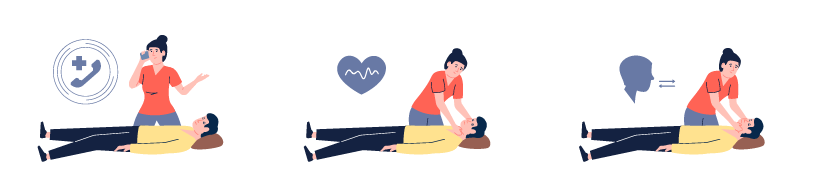
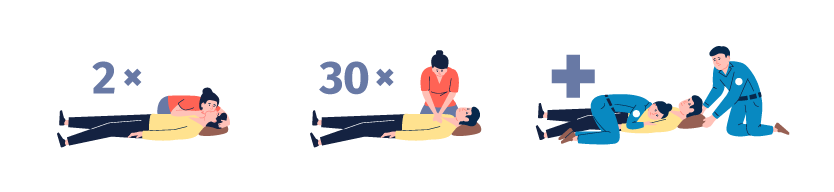
Emergency Room – Save an emergency room (ER) visit for when you need immediate treatment for a serious life-threatening condition such as heavy bleeding, chest pain, major burns, or severe head injuries. These visits are often far more costly than seeing your primary care center and are subject to copay and/or coinsurance. ERs are open 24/7 but come with long wait times since life-threatening emergencies will be seen first. ER visit may also come with ambulance charges that are not covered by insurance or may not be in network.














 Recognizing Signs of Traumatic Stress in Children
Recognizing Signs of Traumatic Stress in Children


 Respiratory Syncytial Virus (RSV)
Respiratory Syncytial Virus (RSV) Sources:
Sources:
