Hobbies can bring a lot of enjoyment into your everyday life, but did you know they can also aid healing and support good mental health?
Hobbies vary by person, but if you’re looking to quiet your mind and provide a distraction from everyday stress, look for something that makes you feel calm, peaceful, restorative, reflective, and quiet (not environmentally per se, but that can quiet intrusive thoughts) to support your relaxation efforts.

Get Outside in Nature
Going outdoors and exploring nature — whether walking, hiking, or running — is a great opportunity to see picturesque locations, challenge yourself physically, release stagnant energy that’s building up, and support your cardiovascular health.
You can customize your activity to meet your energy levels and fitness abilities. In addition to the physical health benefits, these activities can help you shift your focus away from your racing mind and onto your breathing and movement — leaving you with a sense of balance and release.
Mind-Body Exercises
Finding a form of exercise that requires a deliberate focus on your movements, coordination, and breathing can also be physically and mentally beneficial. Yoga and Pilates are excellent examples of exercise routines that can be gentle and healing on the body. They require you to listen to your body, and they can be modified for injury and energy levels.
Dancing is another exercise form that can boost your mood (who doesn’t like moving around to their favorite tunes?) while releasing pent-up stress. You can freestyle dance or focus on specific choreography.


Arts, Crafts & Music
Art and music therapy programs have been gaining popularity in professional medical settings, but you don’t need a prescribed program to benefit from the profound impact of these on your own. Listening to music has proven to reduce anxiety and stress, manage Alzheimer’s and Parkinson’s, reduce depression in the elderly, and improve self-expression and communication.
Art therapy has been shown to be effective and have healing properties in times of crisis, trauma, and grief. Creating art can help regulate emotions and impulses and strengthen identity and self-image.
Volunteering
Volunteering is a way to meet like-minded people in a rewarding setting. There are many volunteer opportunities — you just have to search your community for animal shelters, food banks, local libraries, retirement homes, or even community centers that may be looking for an extra set of hands to help.

Journaling
Journaling is a great way to clear your mind when it’s clouded with buried thoughts. Releasing them from your body and mine so they’re out of your headspace. Even if you spend only 10 minutes a day with a scrap of paper and a pen, journaling you to reflect on your thoughts and emotions so that you don’t carry them with you wherever you go.
Puzzle Games
If you’re looking for something that uses your brain a bit, crosswords, word searches, or sudoku can be a great option. Luckily, there are many of these available on your phone or online, so you can play them on the go!


Hand-related Crafts
Using your hands to knit, crochet, and assemble puzzles can help calm your nerves. A bonus is you can do these activities while conversing or watching TV. The repetitive nature of these can be as complex or simple as you’d like, and you can get lost in designs.














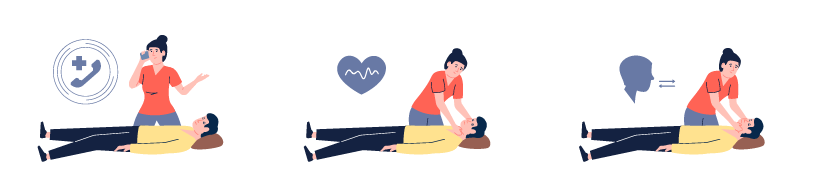
 Recognizing Signs of Traumatic Stress in Children
Recognizing Signs of Traumatic Stress in Children

 Respiratory Syncytial Virus (RSV)
Respiratory Syncytial Virus (RSV) Sources:
Sources: